A SIMPLE act like washing your hands or using an alcohol-based gel to clean them can save a person’s life.
That’s the message specialist infection control staff have been hammering home at Worcestershire Acute Hospital Trust sites in Worcester, Redditch and Kidderminster over the past week.
Making sure hands are free of harmful bacteria is not difficult or time consuming but it’s vital to giving poorly patients the best chance of fighting their ailments and recovery.
The problem with hospitals is that they are full of sick patients and they are also potential breeding ground for infections.
Infection combined with people whose immunity is already depleted, due to their other underlying health conditions, can be fatal.
So the trust has taken the opportunity of reinforcing the importance of hand cleaning to all of its 6,000 staff and hospital visitors too.
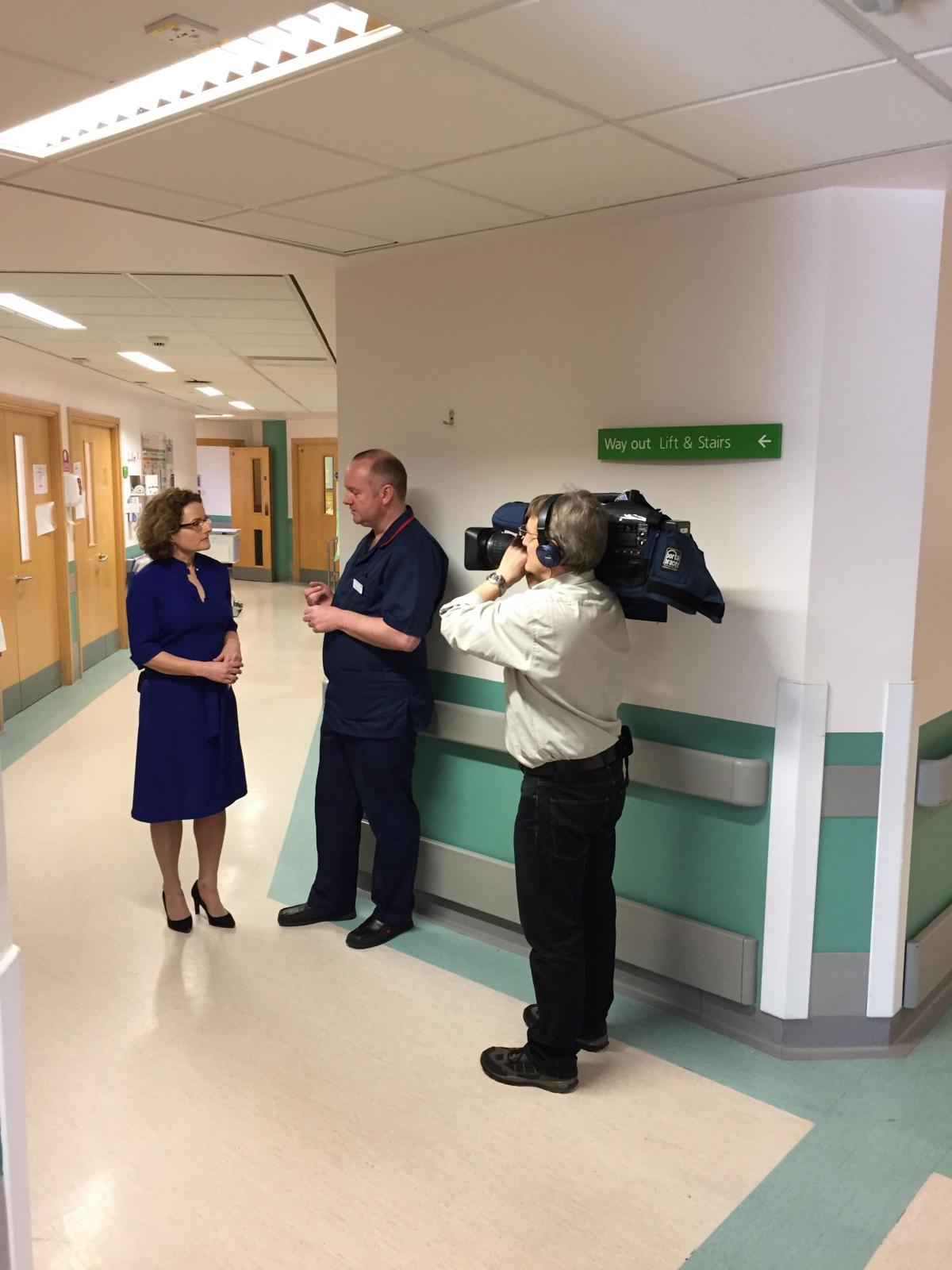
Members of the trust’s infection control team, together with the county’s clinical commission groups’ staff, have been visiting the wards on all sites observing staff practices when it comes to hand hygiene and promoting the importance of taking a few seconds between attending to each patient to clean their hands.
The campaign has also extended to non-front line staff too, as senior managers have also been put through their paces to make sure they use the right technique to clean their hands. This includes rubbing between the fingers and thumbs as well as on the other surfaces.
The trust’s Associate Chief Nurse Infection Control David Shakespeare said: “We have been having a hand hygiene week. Hand hygiene is the single most important thing that a health professional can do to prevent health care acquired infections such as MRSA (meticillin-resistant Staphylococcus aureus) and C. difficile (clostridium difficile).”
He said the team’s observations and audits of the staff use of hand gels and washing their hands between patients had been very good but it is important that staff show patients they are cleaning their hands before attending to them.
“The campaign is about raising the profile of using hand gels and raising the compliance with it. We are also saying that it is OK for patients to challenge staff about it and ask if they have cleaned their hands.”
The team has also offered training on the most thorough way of hand cleaning by employing a Semmelweis scanning machine which shows the areas of the hand that have and have not been cleaned.
The trust is using social media to spread the word about hand hygiene, as well as the intranet, and has put new signs on some wards drawing people attention to the hand gel dispensers. A hand hygiene audit app is also available for staff to use.
David added that the message was the same for any visitors to the hospital. “If people are going to visit the hospital, they should use the alcohol gel as soon as they get in through the door. It is in reception, along corridors and outside and inside the wards.
“I do not think some people know that something as simple as hand hygiene can prevent the spread of infection,” he said.
He also pointed out that although other hospital trusts in the West Midlands had seen a significant rise in the cases of norovirus (one of the most common stomach bugs in the UK which causes diarrhoea and vomiting) this winter, the Worcestershire hospital sites had fewer than in previous years.
“We have done really well this winter although two wards have been closed at Worcestershire Royal recently.” He explained that a ward closure due to norovirus in fact means it is closed to new patient admissions and patients from that ward are not transferred to other wards or health care establishments. Patients infected by the virus might also be isolated within their ward.
The aim is to isolate the infection to stop it spreading and, while visitors can still come in to see patients, it is essential they use the hand wash on entering and leaving the ward.
Once a patient with norovirus has been clear of symptoms for 48 hours, they are generally not infectious and the ward can be reopened.
Another reason for the lower incidence of norovirus this year is likely to be the practice of cleaning all the wards, including touch surfaces like door handles, every day with a chlorine agent. “If there has been an outbreak of infection, we do it more than once a day,” said David.
He said the rigorous attention to hygiene as a normal practice as well as where there is an infection outbreak is part of the hospital’s aims to become a beacon of excellence. “We will continue to measure the staff compliance with hand hygiene best practice to make sure it is sustained after the week’s campaign.”
Panel
According to Public Health England (PHE), the West Midlands as a whole has seen an increase in the number of outbreaks of stomach bugs – including norovirus – this winter. Reports show the incidents are significantly higher than this time last year.
PHE West Midlands is urging people with a stomach bug to phone before visiting their GP or local A&E department.
Dr Helen Carter, Deputy Director for PHE West Midlands, said: “At this time of year we see a lot of diarrhoea and sickness bugs, which are very infectious. So if people feeling unwell with a stomach upset decide to visit their GP, a walk-in centre, or their local A&E, they could be putting a lot of other people at risk of infection and adding significantly to the seasonal pressures already experienced in healthcare settings.
“Norovirus usually leads to mild diarrhoea, vomiting and abdominal or stomach cramps. People generally recover quite quickly from these bugs and there is no specific treatment, apart from drinking plenty of water to avoid dehydration and avoiding reinfection with good hand hygiene – especially before eating and after going to the toilet, along with cleaning touch points and communal areas with a bleach-based cleaner.
“Laboratory reports of norovirus are considerably higher than this time last year and higher than the five-year seasonal average. People feeling unwell can call their GP or NHS111 for advice.
“Over half the outbreaks we’re seeing are in care homes – so it’s really important that staff in those settings seek advice on the phone from their GP surgery before considering transferring people to hospital.
“If someone is seriously unwell and in need of hospitalisation, it is still important to let NHS staff know that the person has an infectious illness, so the correct measures can be taken to avoid spreading the bug to other patients and healthcare workers.”
Dr Kiran Patel, Medical Director for NHS England in the West Midlands, said: “We are asking people not to visit hospitals and care homes to see relatives or friends whilst they have sickness and diarrhoea, or if they have recently experienced these symptoms. This is because people may still carry the virus and infect others up to three days after their symptoms have stopped.
“People concerned about visiting a relative or friend who may be in hospital or living in a care home should speak to the nurse in charge of the hospital ward or phone the care home beforehand for advice.”






Comments: Our rules
We want our comments to be a lively and valuable part of our community - a place where readers can debate and engage with the most important local issues. The ability to comment on our stories is a privilege, not a right, however, and that privilege may be withdrawn if it is abused or misused.
Please report any comments that break our rules.
Read the rules hereLast Updated:
Report this comment Cancel